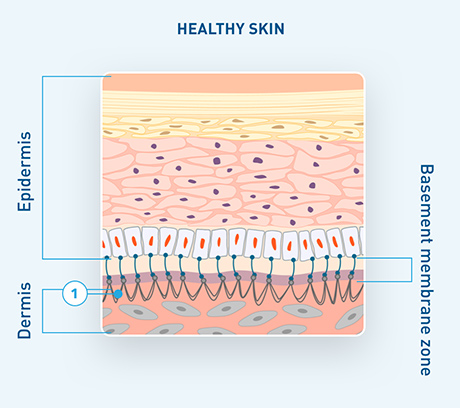
In healthy skin, collagen VII plays a critical role in anchoring fibrils to maintain cohesion between the epidermis and dermis.2,4,6
- Anchoring fibrils
EB refers to a group of genetic blistering disorders characterized by skin fragility due to the separation of connective tissues, ultimately causing blistering and wounds in response to minimal friction or trauma.
Each EB type is defined by unique underlying gene mutations that determine where skin layer separation occurs.
Despite the underlying cause of each EB type being different, all EB types present with similar dermatologic manifestations. Differentiating DEB is critical because patients with DEB require active and vigilant surveillance for progressive and potentially life-threatening external and internal complications.
|
Affected genes |
Affected proteins |
Affected skin layer |
||
|---|---|---|---|---|
Epidermolysis bullosa simplex (EBS) |
CD151, DST, EXPH5, KLHL24, KRT5, KRT14, PLEC |
BPAG1, Exophilin 5, Kelch-like protein 24, Keratin 5, Keratin 14, Plectin, Tetraspanin 24 |
Epidermis |
Occurs in approx. 70% of patients |
Dystrophic epidermolysis bullosa (DEB) |
COL7A1 |
Collagen VII |
Sublamina densa |
Occurs in approx. 25% of patients |
Junctional epidermolysis bullosa (JEB) |
COL17A1, ITGA3, ITGA6, ITGB4, LAMA3, LAMB3, LAMC2 |
Collagen XVII, Integrin α3 subunit, Integrin α6b4, Laminin-332 |
Lamina lucida |
Occurs in approx. 5% of patients |
|
Affected genes |
Affected proteins |
Affected skin layer |
|---|---|---|
|
Affected genes CD151, DST, EXPH5, KLHL24, KRT5, KRT14, PLEC |
Affected proteins BPAG1, Exophilin 5, Kelch-like protein 24, Keratin 5, Keratin 14, Plectin, Tetraspanin 24 |
Affected skin layer Epidermis |
|
Epidermolysis bullosa simplex (EBS)
Occurs in approx. 70% of patients |
||
|
Affected genes |
Affected proteins |
Affected skin layer |
|---|---|---|
|
Affected genes COL7A1 |
Affected proteins Collagen VII |
Affected skin layer Sublamina densa |
|
Dystrophic epidermolysis bullosa (DEB)
Occurs in approx. 25% of patients |
||
|
Affected genes |
Affected proteins |
Affected skin layer |
|---|---|---|
|
Affected genes COL17A1, ITGA3, ITGA6, ITGB4, LAMA3, LAMB3, LAMC2 |
Affected proteins Collagen XVII, Integrin α3 subunit, Integrin α6b4, Laminin-332 |
Affected skin layer Lamina lucida |
|
Junctional epidermolysis bullosa (JEB)
Occurs in approx. 5% of patients |
||
*Kindler EB (KEB) is a very rare type of EB that occurs in <1% of patients and is caused by mutation of the FERMT-1 gene, resulting in mixed separation of multiple layers due to lack of the protein kindlin-1.
Adapted from De Rosa L, Latella MC, Secone Seconetti A, et al. Cold Spring Harb Perspect Biol. 2020.
In healthy skin, collagen VII plays a critical role in anchoring fibrils to maintain cohesion between the epidermis and dermis.2,4,6
In DEB, the mutated COL7A1 gene leads to reduced or absent collagen VII, causing a loss of anchoring fibrils and disrupting the connection between the epidermis and dermis.2-4
This results primarily in skin fragility and blistering of not only the skin but also the mucosa and epithelial lining of organs.3,9
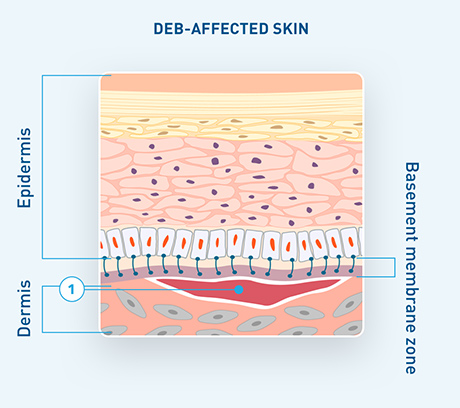
Adapted from De Rosa L, Latella MC, Secone Seconetti A, et al. Cold Spring Harb Perspect Biol. 2020.
DDEB10,11
(Nearly half of patients in the US)
At least 1 parent is affected
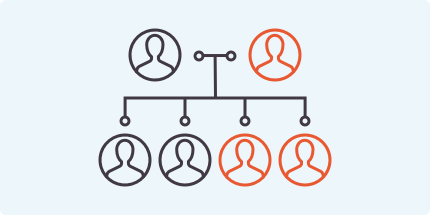
RDEB10,11
(Nearly half of patients in the US)
Neither parent is affected, but both are carriers

In some cases, DEB can occur de novo, confirmed by the absence of an affected COL7A1 gene in both parents.12
Both DEB subtypes can present with similar dermatologic symptoms, a range in severity, and potential for serious complications. Regardless of severity, both DDEB and RDEB share an increased risk for complications, including squamous cell carcinoma (SCC).7,9,13-15
DEB can easily be missed or misdiagnosed when looking at symptoms alone1,7,16,17
References: 1. Bruckner AL, Losow M, Wisk J, et al. The challenges of living with and managing epidermolysis bullosa: insights from patients and caregivers. Orphanet J Rare Dis. 2020;15(1):1. doi:10.1186/s13023-019-1279-y 2. Denyer J, Pillay E, Clapham J. Best practice guidelines for skin and wound care in epidermolysis bullosa. Wounds International. May 3, 2017. Accessed June 13, 2022. https://www.woundsinternational.com/resources/details/best-practice-guidelines-skin-and-wound-care-in-epidermolysis-bullosa 3. Fortuna G, Aria M, Cepeda-Valdes R, Trevino MGM, Salas-Alanís JC. Pain in patients with dystrophic epidermolysis bullosa: association with anxiety and depression. Psychiatry Investig. 2017;14(6):746-753. doi:10.4306/pi.2017.14.6.746 4. Eichstadt S, Tang JY, Solis DC, et al. From clinical phenotype to genotypic modelling: incidence and prevalence of recessive dystrophic epidermolysis bullosa (RDEB). Clin Cosmet Investig Dermatol. 2019;12:933-942. doi:10.2147/CCID.S232547 5. Condorelli AG, Dellambra E, Logli E, Zambruno G, Castiglia D. Epidermolysis bullosa–associated squamous cell carcinoma: from pathogenesis to therapeutic perspectives. Int J Mol Sci. 2019;20(22):5707. doi:10.3390/ijms20225707 6. De Rosa L, Latella MC, Secone Seconetti A, et al. Toward combined cell and gene therapy for genodermatoses. Cold Spring Harb Perspect Biol. 2020;12(5):a035667. doi:10.1101/cshperspect.a035667 7. Has C, Liu L, Bolling MC, et al. Clinical practice guidelines for laboratory diagnosis of epidermolysis bullosa. Br J Dermatol. 2020;182(3):574-592. doi:10.1111/bjd.18128 8. Has C, Bauer JW, Bodemer C, et al. Consensus reclassification of inherited epidermolysis bullosa and other disorders with skin fragility. Br J Dermatol. 2020;183(4):614-627. doi: 10.1111/bjd.18921 9. Fine J-D, Mellerio JE. Extracutaneous manifestations and complications of inherited epidermolysis bullosa: part I. Epithelial associated tissues. J Am Acad Dermatol. 2009;61:367-384. doi:10.1016/j.jaad.2009.03.052 10. Fine J-D. Epidemiology of inherited epidermolysis bullosa based on incidence and prevalence estimates from the National Epidermolysis Bullosa Registry. JAMA Dermatol. 2016;152(11):1231-1238. doi:10.1001/jamadermatol.2016.2473 11. Slide show: how genetic disorders are inherited. Mayo Clinic. Updated February 15, 2020. Accessed June 13, 2022. https://www.mayoclinic.org/tests-procedures/genetic-testing/multimedia/genetic-disorders/sls-20076216?s 12. Autosomal dominant. Medlineplus.gov. Accessed June 13, 2022. https://medlineplus.gov/ency/article/002049.htm 13. Das BB, Sahoo S. Dystrophic epidermolysis bullosa. J Perinatol. 2004;24(1):41-47. doi:10.1038/sj.jp.7211019 14. Fine J-D, Bruckner-Tuderman L, Eady RAJ, et al. Inherited epidermolysis bullosa: updated recommendations on diagnosis and classification. J Am Acad Dermatol. 2014;70(6):1103-1126. doi:10.1016/j.jaad.2014.01.903 15. EB in Depth. Debra of America. Accessed June 13, 2022. https://debra.org/about-eb/eb-depth 16. Kao C-H, Chen S-J, Hwang B, Yang A-H, Hsu C-Y, Huang C-H. Junctional epidermolysis bullosa. J Chin Med Assoc. 2006;69(10):503-506. 17. Tabor A, Pergolizzi JV Jr, Marti G, Harmon J, Cohen B, Lequang JA. Raising awareness among healthcare providers about epidermolysis bullosa and advancing toward a cure. J Clin Aesthet Dermatol. 2017;10(5):36-48.